
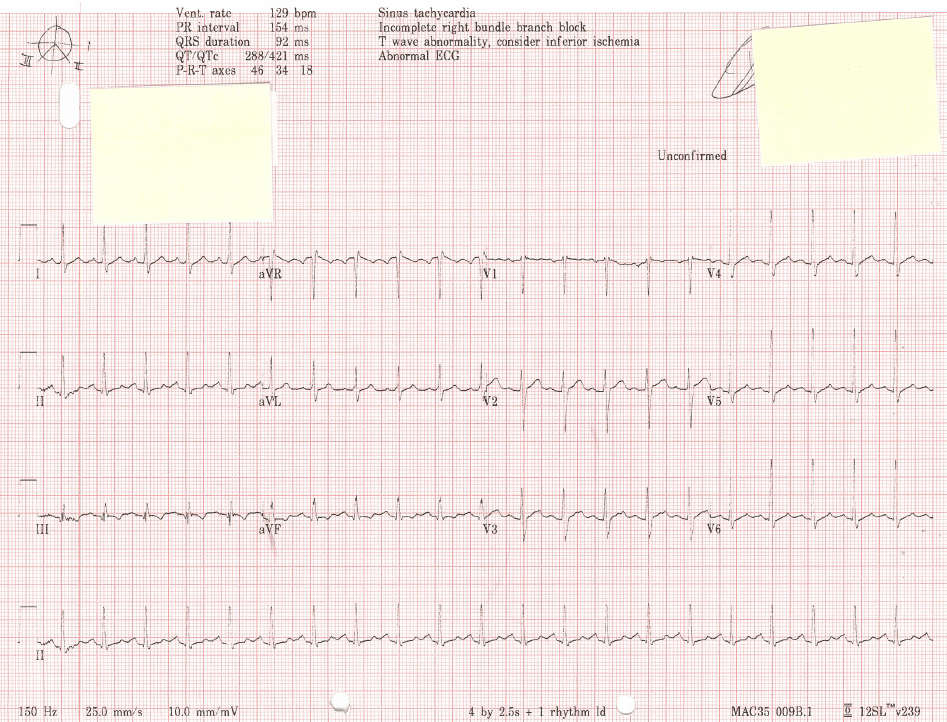
An ECG reading with this pattern shows: a pronounced S wave in lead 1 a pronounced Q wave. Right ventricular (RV) strain pattern was significantly more commonly in patients than controls, 11.1% vs 2.6% (sensitivity 11.1%, specificity 97.4% OR 4.58, 95% CI 1.63 to 15.91 p=0.002), particularly in those with large clot load, 17.1% vs 2.6% (sensitivity 17.1%, specificity 97.4% OR 7.55, 95% CI 1.62 to 71.58 p=0.005).Īn ECG showing RV strain in a breathless patient is highly suggestive of PE. The S 1 Q 3 T 3 pattern is a common ECG finding when a PE is present. Right bundle branch block (9.0%), atrial dysrhythmias (10.1%) and clockwise rotation (20.1%) occurred more frequently but were also common in controls. T wave inversion in the anterior leads has been reported in many studies as the most common ECG finding among patients with PE, particularly massive PE. S1Q3T3 (3.7%), P pulmonale (0.5%) and right axis deviation (4.2%) were infrequent findings. Various ECG abnormalities are reported in PE patients however, the ECG findings lack sensitivity and specificity for PE. The most common ECG findings in PE are tachycardia and nonspecific ST-segment and T-wave changes, S1Q3T3 pattern, right ventricular strain, and new incomplete right bundle branch block are uncommon. The most common ECG abnormality in patients with PE was sinus tachycardia (28%). We scored each ECG for the presence or absence of eight features that have been reported to occur more commonly in PE.Ģ0%-25% of patients with PE, including those with large clot load, had normal ECGs. We considered those with large (n=76) and small (n=113) clot load separately. We matched these for age☓ years with 189 controls with suspected PE whose CTPA was negative. We identified 189 consecutive patients with suspected PE whose CT pulmonary angiogram (CTPA) was positive for a first PE and for whom an ECG taken at the time of presentation was available. Retrospective case-control study in a district general hospital setting. All rights reserved.To establish the diagnostic value of prespecified ECG changes in suspected pulmonary embolism (PE). Approximately one-quarter of patients will have a new sinus tachycardia, and approximately one-quarter will have no change in their ECG.ĮCG changes with pulmonary embolism electrocardiographic changes electrocardiographic changes with pulmonary embolism pulmonary embolism.Ĭopyright © 2016 Elsevier Inc.
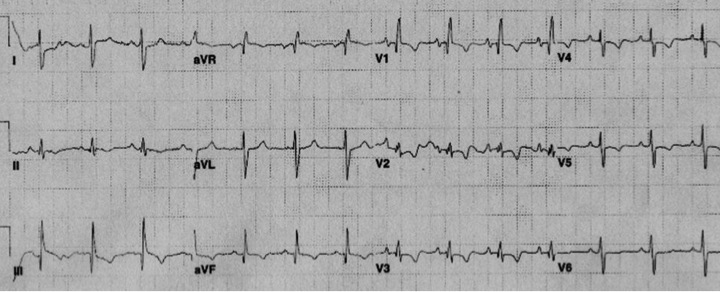
The most common ECG changes when compared with previous ECG in the setting of PE are T wave inversion and flattening, most commonly in the inferior leads, and occurring in approximately one-third of cases. In 24.1% of patients, no new ECG changes were noted, with this finding more likely to occur in patients younger than 60 years. A new sinus tachycardia occurred in 27.3% of cases. New T wave flattening, also most commonly in the inferior leads, was the second most common change, occurring in 29.5%. New T wave inversions, commonly in the inferior leads, were the most common change found, occurring in 34.4% of cases.
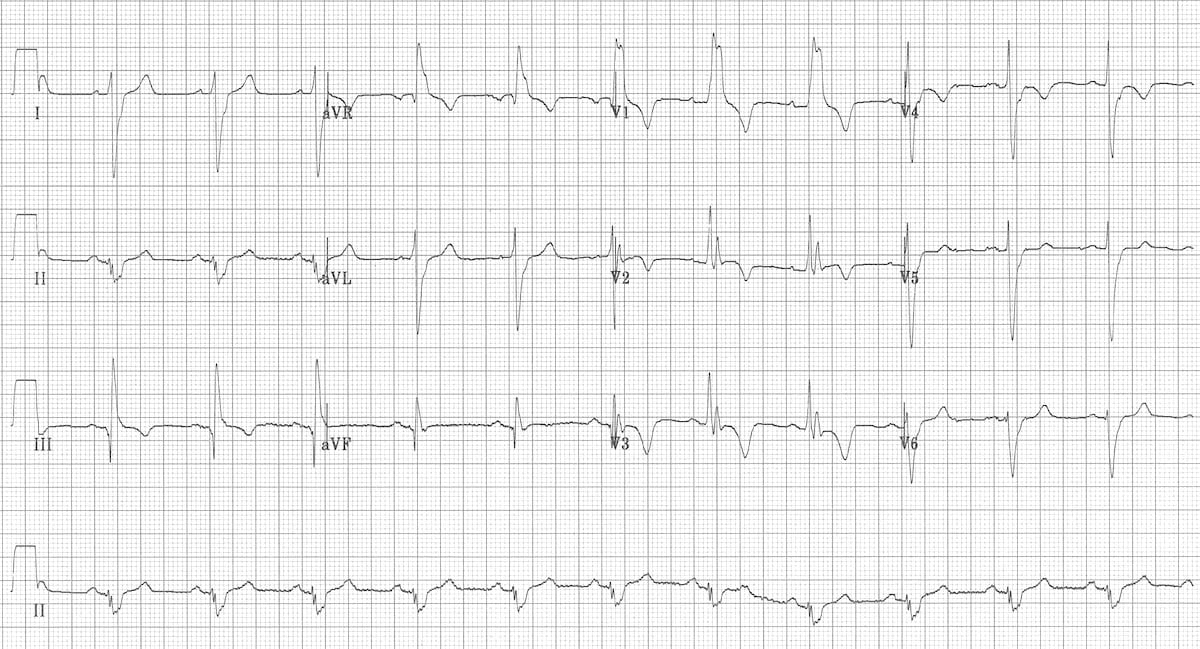
Each patient's presenting ECG was compared with their most recent ECG obtained before diagnosis of PE.Ī total of 352 cases were reviewed. Our aim was to identify the most common ECG changes in patients with known PE when their ECGs were compared with their previous ECGs.Ī retrospective chart review of patients diagnosed with PE in the emergency department was performed. Previous studies have evaluated ECG patterns predictive of pulmonary embolism (PE) at the time of PE diagnosis, though none have examined ECG changes in these patients when compared with their previous ECGs. The electronic medical record is a relatively new technology that allows quick review of patients' previous medical records, including previous electrocardiograms (ECGs).


 0 kommentar(er)
0 kommentar(er)
